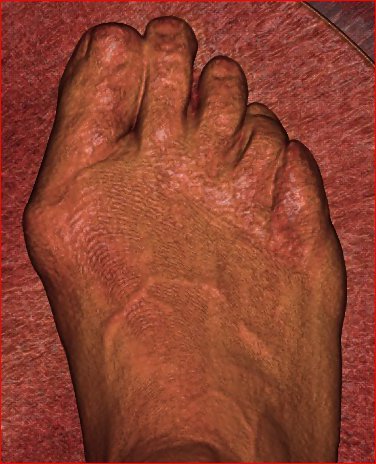
My mentor Dr. William Hamilton of the Hospital for Special Surgery always said, “Bunions are a big deal”. After practicing orthopaedic surgery for more than a decade, I have come to realize that he was not wrong. Many patients come in to P.O.W. thinking a bunion is just a growth of tissue or bone that needs to just be removed. At times, a “pseudobunion” or arthritic spur may appear this way and, yes, that can just be removed. However, a true bunion or what is technically knowns as a “Hallux Valgus” deformity is much more complex.
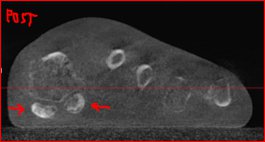
I like to describe a bunion as a foot trying to become a hand. As the first metatarsal moves away from the second, the big toe starts to rotate into a position that is much like a thumb! This is a complex problem that involves rotation of the bones, instability of joints, and malalignment of tendons. In more severe cases, a bunion involves instability of the metatarsal where it meets the bones of the midfoot. This is instability of the 1st tarsometatarsal joint (indicated by the red arrow). This is much like the motion seen at the 1st carpometacarpal joint of the thumb that allows for grasping or opposition. In a normal foot, the 1st tarsometatarsal joint is relatively stable.


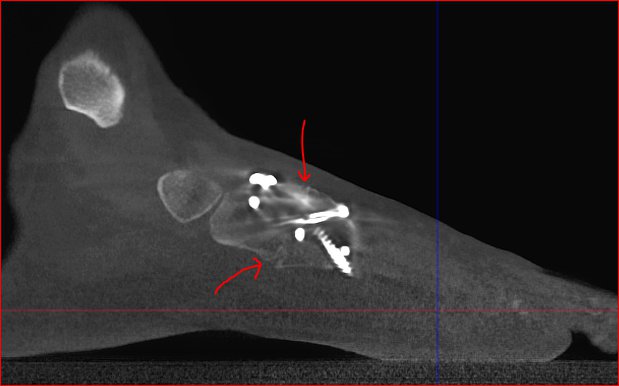
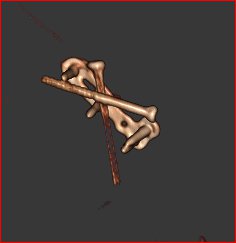
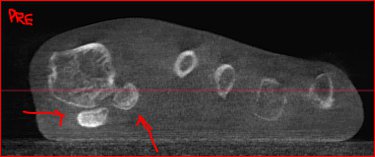
Whereas plain x-rays, as taken at UPMC and AHN, are two-dimensional, the added value of the PedCAT CT scanner at P.O.W. is that we see all problems of the foot and ankle in a 3-dimensional way. The complexity of a bunion, especially when severe, requires attention to the alignment of the metatarsals, the sesamoid bones, the toe phalanges, and the tendons. The PedCAT helps us to see and appreciate the alignment of all of these structures.
Paul W. Lapidus described the bunion deformity in a three-dimensional way back in 1934 popularizing a procedure described by Albrecht in 1911. This description emphasized the deviation of the 1st metatarsal from the 2nd metatarsal and suggested that this be corrected at the 1st tarsometatarsal joint. Since this joint is typically stable in the foot, fusing this joint so that it could no longer move in an unstable bunion is thought to be the best way to correct the deformity.
Don’t fear the word “fusion” as the 1st tarsometatarsal joint is a non-essential joint that, when fused, does not cause any significant loss of mobility. (unlike a fusion at the big toe joint, the metatarsophalangeal joint, which is more limiting)
Of particular importance in correcting a severe bunion is stabilizing the 1st tarsometatarsal joint along with correcting rotation of the metatarsal in such a way that the sesamoid bones are properly reduced under the big toe. These bones normally live in their grooves under the metatarsal head at the big toe. When they move out of their grooves this becomes a very unstable situation propagating the bunion deformity. This causes weight to be transferred into the 2nd toe and often causes a hammertoe to form. Hammertoe deformities are very often due to a bunion deformity. Thus, correcting a hammertoe without correcting a bunion deformity, is a bad idea.




At P.O.W. we have been performing the modified-Lapidus bunionectomy for over a decade. In recent years, the proprietary device called the Lapiplasty® was developed by Treace Medical to help surgeons make cuts that they did not feel they could make without guidance. The company has also developed large plates to stabilize the joint with hopes that it would allow people to walk faster after this surgery. However, due to the inherently unstable nature of the 1st tarsometatarsal joint, one must allow for adequate healing time before bearing weight or the plates could break before the bone heals. This usually requires 4 to 6 weeks of protection in a boot after the initial post-operative dressings.
With the PedCAT CT scanner at P.O.W., you can be assured that your bone has healed so that you do not risk breaking your hardware or having a failure of your fixation. The metal artifact reduction feature helps us to be certain that the hardware remains intact and that the bone is healed before you return to dancing, running, or hiking the trails.